Taking care of an aging parent can be overwhelming, but creating a consistent daily routine can make life easier for both of you. A structured plan helps seniors feel secure, improves their physical and mental health, and reduces caregiver stress. Here’s how to build a practical daily care routine in 7 steps:
- Assess Needs and Preferences: Understand your parent’s abilities, challenges, and personal habits. Focus on Activities of Daily Living (ADLs) like bathing and eating, and Instrumental Activities of Daily Living (IADLs) like managing medications and finances.
- Create a Simple Schedule: Divide the day into morning, afternoon, and evening blocks. Include regular times for meals, hygiene, and rest.
- Focus on Core Care Areas: Prioritize hygiene, nutrition, hydration, and physical/mental activities. Use tools like adaptive clothing or pre-cut vegetables to simplify tasks.
- Address Health Conditions and Safety: Tailor routines for specific needs like dementia or arthritis. Make the home safer with grab bars, non-slip mats, and proper lighting.
- Coordinate with Family and Caregivers: Share responsibilities among family members and use tools like shared calendars for communication.
- Test and Adjust: Start small, observe what works, and tweak the routine as needed. Flexibility ensures the schedule fits your parent’s changing needs.
- Take Care of Yourself: Schedule breaks, use respite care, and prioritize your own health to avoid burnout.
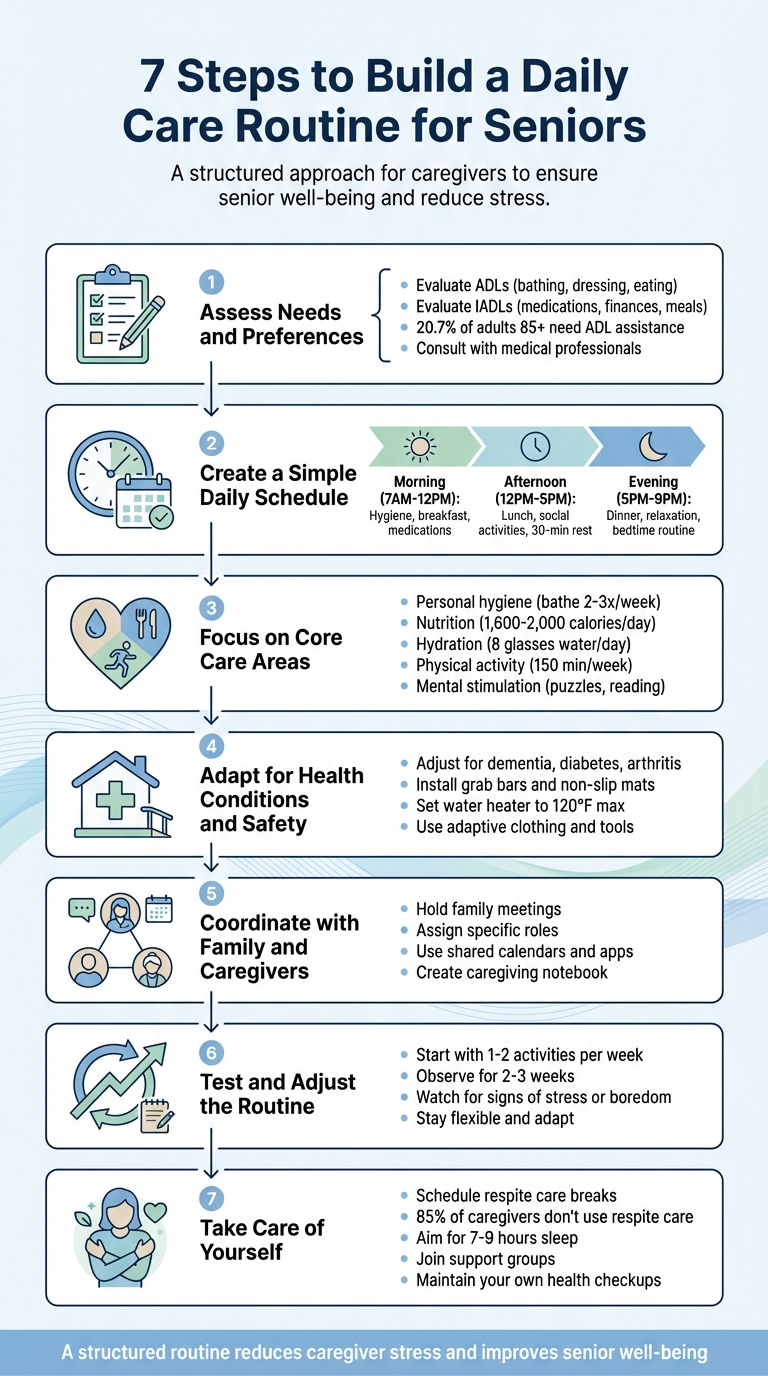
7 Steps to Build a Daily Care Routine for Seniors
Importance Of Elderly Health Routines to Help Aging Parents Stay Healthy and Active At Home
Step 1: Assess Your Parent’s Needs and Preferences
Before diving into creating a routine, it’s crucial to understand your parent’s current abilities and priorities. Take a clear-eyed look at what they can handle independently, where they might need support, and what matters most to them. The idea isn’t to take over their life – it’s about finding the right balance of assistance.
Evaluate Activities of Daily Living (ADLs) and Instrumental Activities (IADLs)
Start by observing how your parent manages day-to-day tasks. Activities of Daily Living (ADLs) include the basics like bathing, dressing, using the bathroom, moving between a bed and chair, managing continence, and eating. On the other hand, Instrumental Activities of Daily Living (IADLs) cover more complex responsibilities, such as handling finances, organizing medications, preparing meals, shopping, cleaning, doing laundry, arranging transportation, and staying connected.
Generally, IADLs are the first to show signs of decline, often pointing to early cognitive challenges, while ADLs tend to be affected later. For instance, research shows that around 20.7% of adults aged 85 or older require assistance with ADLs, compared to only 3.4% of those aged 65 to 74. Keep an eye out for warning signs like stacks of unopened mail, noticeable weight loss, or wearing the same clothes for days.
"If someone is concerned about their mom, then knowing how they’re doing with ADLs is important. It can educate a person and take them from feeling like ‘Mom needs help, I’m worried,’ to be able to answer questions like, ‘OK, where does she need help?’" – Dr. Leslie Kernisan, Geriatrician
Take your time with this assessment. Observe over a few days and gather input from other family members. Instead of simply asking if they can or can’t do something, evaluate their abilities on a scale – "sometimes", "a little bit", or "often". This approach offers a more nuanced understanding, helping you avoid overestimating or underestimating their needs. A thorough assessment like this sets the stage for building a realistic and effective care routine.
Include Personal Preferences and Existing Routines
Your parent’s preferences play a key role in designing a routine they’ll actually embrace. Learn about their natural rhythms – when they like to wake up and go to bed, whether they prefer a morning shower or an evening bath, and what meals or snacks they enjoy most. These familiar habits provide stability and reduce the chances of resistance.
Also, think about the activities that bring them joy and a sense of purpose. Maybe it’s reading the newspaper over coffee, attending religious services, or gardening. Incorporating these habits into their daily schedule helps maintain their identity and self-esteem. Plan more demanding tasks, like doctor visits or physical therapy, during their peak energy times – often in the morning.
"The type of activity and how well it’s completed are not as important as the joy and sense of accomplishment the person gets from doing it." – Alzheimer’s Association
Consult with Medical Professionals
Schedule a check-up with your parent’s doctor to identify any health issues that might be affecting their abilities. Changes in their ability to manage daily tasks could signal underlying problems like infections, cognitive decline, or chronic conditions that require attention.
"Alignment on Activities of Daily Living is critical to having an accurate care plan. If your physician doesn’t realize there’s a functional impairment, then the care plan they create for your loved one may not be in line with their abilities." – Dr. Leslie Kernisan, Geriatrician
Ask the doctor to use standardized tools like the Katz Index (for assessing basic self-care) or the Lawton IADL Scale (for more complex tasks). These assessments only take 10 to 15 minutes and provide valuable insights. Be ready to share specific examples of changes you’ve noticed – like near-misses while driving, unpaid bills piling up, or frequent falls. The doctor may also recommend occupational or physical therapy to suggest exercises or adaptive devices like walkers or grab bars. If your parent qualifies for long-term care insurance or VA benefits, you’ll likely need formal documentation proving they require help with at least two ADLs. This professional input will be essential for shaping the care plan and daily schedule.
Step 2: Create a Simple Daily Schedule
After understanding your parent’s needs and preferences, the next step is to craft a daily schedule that brings structure to their day. Think of it as a flexible guide – something that provides consistency while allowing room for spontaneity.
"A planned day allows you to spend less time trying to figure out what to do, and more time on activities that provide meaning and enjoyment." – Alzheimer’s Association
Here’s how you can break the day into manageable segments.
Divide the Day into Key Time Blocks
Organizing the day into morning, afternoon, and evening blocks can make planning easier. Each block can focus on specific activities, such as hygiene and exercise in the morning, social engagement in the afternoon, and relaxation in the evening.
- Morning (7:00 AM–12:00 PM): Begin with a consistent wake-up time, followed by hygiene, a healthy breakfast, medications, and light physical or mental activities.
- Afternoon (12:00 PM–5:00 PM): Schedule lunch, social activities like phone calls or visits, and errands. Include a short rest period, such as a 30-minute nap, to recharge and help manage late-day fatigue or sundowning.
- Evening (5:00 PM–9:00 PM): Focus on winding down with dinner, calming activities, nighttime hygiene, and a set bedtime routine.
| Time Block | Primary Focus | Example Activities |
|---|---|---|
| Morning (7:00 AM–12:00 PM) | Orientation & Energy | Hygiene, breakfast, medications, exercise, puzzles |
| Afternoon (12:00 PM–5:00 PM) | Nutrition & Social | Lunch, phone calls, errands, 30-minute rest |
| Evening (5:00 PM–9:00 PM) | Wind-down | Dinner, relaxation, night hygiene |
| Night (9:00 PM onwards) | Restorative Sleep | Consistent bedtime, sleep preparation |
This structure not only organizes the day but also helps establish a comforting routine.
Build the Routine Around Regular Activities
Anchor the schedule with consistent activities like meals, medications, and bedtime. Predictable routines can provide a sense of security, especially for seniors with dementia. Routines tap into long-term procedural memory, which often stays intact longer than short-term memory.
"Once a routine becomes a natural part of their life, they’ll be more likely to go with the flow and won’t feel as if you’re suddenly forcing them to do a specific activity." – Connie Chow, Founder, DailyCaring.com
To make the schedule easier to follow, post it somewhere visible, like on a whiteboard or a large-print calendar in a central area, such as the kitchen. Keeping bedtimes within a few hours after sunset can also align with the body’s natural rhythms. While structure is important, don’t hesitate to adjust the plan for unexpected opportunities or needs. Flexibility keeps the routine practical and enjoyable.
Step 3: Focus on Core Care Areas
Make sure your parent’s daily routine includes essential care activities that promote their health and well-being. These key areas are the backbone of any effective caregiving plan and should be prioritized consistently.
Personal Hygiene and Grooming
Maintaining a regular hygiene routine is crucial for preventing infections, preserving dignity, and keeping an eye on overall health. Aim for bathing 2–3 times a week, and on non-bath days, opt for sponge baths, focusing on areas like the face, hands, feet, underarms, and private regions. To prevent falls, use safety measures like rubber bathmats, grab bars, and bath chairs, and always check the water temperature before starting.
Oral care is equally important. Encourage brushing twice daily – morning and evening – and include flossing and a mouthwash rinse once a day. For older adults with limited mobility, tools like electric or long-handled toothbrushes can make the process easier. Dressing in clean, weather-appropriate clothing each day not only ensures comfort but also supports a sense of self-respect. To simplify the process, lay out clothes in the order they should be put on and consider adaptive clothing with Velcro fasteners or large zippers instead of small buttons.
"The main goal is to find the balance of letting the person be as independent as possible while providing support when needed." – National Institute on Aging
Don’t forget regular grooming tasks like hair care, nail trimming, and shaving. Use an electric razor for added safety, and take the opportunity during these routines to check for skin issues such as irritations, sores, or dryness. For seniors dealing with incontinence, creating a toileting schedule – every three hours, for instance – can help prevent accidents and protect skin health.
Nutrition and Hydration
Balanced meals and staying hydrated are essential for sustaining energy, aiding digestion, and supporting mental clarity. Encourage drinking 8 glasses of water a day, pairing hydration with regular activities like taking medications or after light exercise. While older adults may need fewer calories – about 1,600 to 1,800 daily for women over 50 and 2,000 for men – they still require the same or even higher amounts of vital nutrients like protein, fiber, and vitamin B12.
Planning meals ahead of time can reduce stress and ensure variety. If manual dexterity is a challenge, use pre-cut or frozen vegetables. Incorporate protein-rich foods like seafood, beans, fortified soy products, or dairy to help maintain muscle strength. Since taste and smell often decline with age, enhance flavors using herbs, citrus, or spices instead of salt.
"As people get older, they are doing less high-energy calorie-burning tasks. They need fewer calories, but the same nutrients." – Dr. Valentina Remig, Registered Dietician
Eating alone can diminish appetite and lead to malnutrition, a concern for 5–10% of seniors living at home and up to 60% of those hospitalized. Whenever possible, share meals with friends or family to make dining more enjoyable. For seniors with dementia, simplify meals by offering finger foods and limiting options to avoid overwhelming them.
Physical and Mental Activities
Physical movement and mental engagement are vital for maintaining independence and reducing feelings of isolation. Encourage 150 minutes of moderate aerobic activity weekly, along with muscle-strengthening exercises twice a week. Even a daily 30-minute walk can do wonders for mood and energy levels.
Activities that improve balance, such as Tai Chi, yoga, or chair yoga, can help prevent falls. Meanwhile, mental exercises – like reading, solving puzzles, or picking up a new skill – can sharpen cognitive abilities. Everyday tasks like gardening or light cleaning can also be used as opportunities for movement and a sense of accomplishment.
"Structure in daily routines can significantly impact the psychological well-being of seniors, offering a myriad of benefits that extend beyond mere scheduling to deeply affect mental health." – Melanie Donohue, LCSW, Founder of Blue Moon Senior Counseling
Social interaction is equally important. Schedule regular calls, visits to community centers, or group activities like fitness classes to combat loneliness and support emotional health. To make new habits stick, link them to existing ones – such as stretching before bed, taking a short walk after breakfast, or working on a puzzle during an afternoon break.
| Activity Category | Examples | Primary Benefit |
|---|---|---|
| Physical | Walking, Tai Chi, Chair Yoga, Swimming | Strength, balance, fall prevention |
| Mental | Puzzles, Reading, Learning a Language | Cognitive stimulation and memory |
| Social | Volunteering, Senior Centers, Group Games | Emotional support and reduced isolation |
| Relaxation | Meditation, Deep Breathing, Music | Stress relief and better sleep |
For more expert guidance and detailed resources on managing your parent’s care routine, visit ElderHonor (https://elderhonor.com).
Next, in Step 4, we’ll explore how to tailor these routines to specific health conditions and ensure safety at home.
Step 4: Adapt the Routine for Health Conditions and Safety
Once you’ve established the core care activities, it’s time to address your parent’s specific health needs and ensure their home is as safe as possible. This step is all about tailoring the routine to their medical conditions and making adjustments that support their safety and well-being. After all, what works for someone with arthritis might not be suitable for a parent managing dementia or diabetes.
Adjust for Medical Conditions
For dementia, sticking to a consistent routine can ease anxiety and improve orientation [4, 30]. Start each day with "reality orientation" by reviewing the date, weather, and the day’s plan using tools like a large calendar or whiteboard. This method leverages long-term memory, which tends to stay intact longer than short-term memory. If your parent experiences sundowning (agitation in the late afternoon), try closing curtains to minimize confusing shadows and ensure rooms are brightly lit.
"Setting a routine and implementing a visible plan can provide a sense of reassurance, stability, and safety." – The Center for Brain/Mind Medicine
For diabetes, timing is everything. Use pill organizers and set phone reminders to ensure medications and meals are taken on schedule [9, 21].
For arthritis or mobility challenges, small changes can make a big difference. Swap out buttons and zippers for Velcro fasteners on clothes and shoes [21, 31]. Replace manual razors with electric ones to accommodate limited hand strength. If utensils are hard to manage, serve nutritious finger foods that are easy to handle while still meeting dietary needs [21, 31].
| Condition | Routine Modification | Safety/Support Tool |
|---|---|---|
| Dementia | Morning orientation; music therapy | Whiteboards or large calendars |
| Diabetes | Timely medications and meals [9, 21] | Pill organizers; phone reminders |
| Arthritis | Gentle stretching; adaptive clothing | Velcro fasteners; electric razors [21, 31] |
| Mobility Issues | Regular rest breaks | Non-slip mats; grab bars; nightlights [9, 31] |
Addressing medical needs is just one part of the equation. Next, it’s essential to ensure the home is a safe space for your parent.
Improve Home Safety
Preventing falls and other accidents starts with a few key precautions. Install grab bars in bathrooms near toilets and showers, and use non-slip mats to reduce the risk of slipping [9, 31]. A shower seat can also provide extra stability and help conserve energy during bathing. Keep walking paths free of clutter and ensure they’re well-lit with nightlights [9, 31]. To avoid scalding, set the water heater to a maximum of 120°F (48.9°C).
In the kitchen, turn pot handles inward to prevent accidental spills, and store commonly used items at waist level to reduce the need for bending or reaching. Replace traditional doorknobs and faucets with lever-style handles that are easier to use for those with limited grip strength. For stairs, install handrails on both sides and use contrasting colors on stair treads to improve visibility for individuals with low vision. Motion-sensor lights along outdoor paths and stairways can also help ensure safe navigation after dark.
"A simple checklist could be the difference between a fall and a phone call." – JubileeTV
Keep emergency contact numbers near every phone, and consider investing in a medical alert pendant or fall detection system for added security. These adjustments not only create a safer living environment but also help maintain your parent’s sense of independence and dignity.
sbb-itb-48c2a85
Step 5: Coordinate with Family and Caregivers
Once you’ve adjusted routines for health and safety, it’s time to focus on building a strong support system. Sharing responsibilities among family members, professionals, and community resources is key to avoiding burnout and ensuring consistent care.
Assign Roles and Responsibilities
Start with a family meeting that includes your parent and any caregivers. Use this time to discuss current needs and plan for future ones before emergencies force rushed decisions. Designate one primary caregiver to oversee daily tasks and act as the main contact for doctors and hired help. Others can take on roles that match their strengths and schedules.
Sharing responsibilities is non-negotiable. Match tasks to the skills and availability of each person. For instance, a tech-savvy family member might manage communication apps and shared calendars, while someone detail-oriented could handle medical bills and insurance paperwork. Those who live nearby can take on tasks like grocery shopping or driving to appointments, while relatives farther away can coordinate schedules, research resources, or provide emotional support. Keep in mind that non-professional caregivers are typically limited to prompting medication reminders rather than administering them.
| Task Category | Specific Responsibilities | Ideal For |
|---|---|---|
| Administrative | Paying bills, handling insurance claims | Organized, detail-oriented members |
| Logistical | Transportation, grocery shopping | Local family members |
| Communication | Managing updates, apps, and calendars | Tech-savvy members |
| Direct Care | Bathing, dressing, medication prompting | Primary caregiver or professionals |
| Emotional/Social | Phone calls, visits, playing games | Long-distance or busier members |
Once roles are assigned, it’s easier to maintain a consistent care plan. Clear communication is essential to keep everyone on the same page.
Use Shared Tools for Communication
Group texts alone won’t cut it. Create a caregiving notebook – either digital or paper – that includes your parent’s medical history, doctor contacts, medication details, and financial information. This resource should be accessible to all caregivers and can even be part of a formal care contract if you’re hiring additional help.
Consider using smartphone apps designed for caregiving to organize schedules, share updates, and assign tasks. Alternatively, place a whiteboard or large paper calendar in a central location in your parent’s home. This allows everyone – family, caregivers, and in-home aides – to see the daily schedule at a glance.
If family resources are stretched thin, look into community services like the Eldercare Locator (800-677-1116) for local support. You might also hire a geriatric care manager to help with more complex needs.
For additional tools and guidance, visit ElderHonor to access resources like the ElderHonor Toolkit and personalized coaching. These can help strengthen your caregiving network and make the process smoother for everyone involved.
Step 6: Test and Adjust the Routine
No routine is perfect from the start. Think of your initial schedule as a rough draft. The Alzheimer’s Association sums it up perfectly: "Planning activities for a person with dementia works best when you continually explore, experiment and adjust". This principle applies to all seniors, not just those facing cognitive challenges.
Start Small and Make Gradual Changes
Avoid the temptation to overhaul everything at once. Instead, introduce one or two activities each week. For instance, you might begin with morning hygiene and a short walk after breakfast. Once these become part of the daily rhythm, you can add other elements like an afternoon social activity or evening medication reminders. Too many changes at once can lead to confusion and resistance.
Plan demanding tasks during their most alert hours. If your loved one is sharpest between 9:00 a.m. and 11:00 a.m., use that time for activities like bathing or doctor’s appointments. Save lighter activities – watching TV, listening to music, or chatting – for periods when their energy tends to dip. Observe how the routine works in real life and adjust based on what you notice.
Observe and Adjust as Needed
Pay attention to how your parent responds. Signs like boredom, distraction, or irritability may mean an activity is too difficult, too long, or just not the right fit. If they seem agitated, switch gears to something else. The goal is to create moments of enjoyment and accomplishment.
Keep a log for 2–3 weeks to track what works and what doesn’t. Note if your parent is sleeping better, eating well, or showing signs of frustration. Skipped meals, hidden food, or excessive daytime sleep could signal the need for changes. Also, watch for signs of social withdrawal, which has been linked to a 29% higher risk of all-cause mortality and a 59% higher risk of functional decline in older adults.
Be patient – it’s normal for some activities to work one day and fall flat the next. The routine should act as a supportive guide for the day, not a rigid set of rules. If grandchildren visit, embrace the spontaneity. However, if unexpected changes cause anxiety, a predictable schedule may be more comforting. Fine-tuning the routine takes time, but it’s worth the effort to create a structure that works.
Step 7: Take Care of Yourself as a Caregiver
Once you’ve fine-tuned your caregiving routine, it’s crucial to remember that your own health and well-being matter just as much. The National Institute on Aging emphasizes this point: "Taking care of yourself is one of the most important things you can do as a caregiver". Yet, statistics show that 85% of caregivers don’t utilize respite care, and 63% report feeling stressed in their caregiving role. This kind of neglect can lead to serious health issues, including sleep problems, high blood pressure, chronic illnesses, and even a shorter lifespan. Prioritizing your health isn’t selfish – it’s necessary to continue providing the best care possible.
Schedule Breaks and Respite Care
Even if you’re providing upwards of 24 hours of care each week, it’s still possible – and essential – to schedule breaks. Respite care provides you with time to recharge, whether that’s for a few hours or a few days. Options include in-home aides, adult day care programs, or short-term stays at nursing facilities. The CDC puts it plainly: "To be an effective caregiver, you must take care of yourself. The person you are caring for is counting on you".
Look for natural breaks in your parent’s routine to carve out time for yourself. For instance, if your parent naps daily from 2:00 p.m. to 4:00 p.m., use that window to take a walk, run errands, or simply relax. If you’re enlisting help from family or hiring professionals, provide a written schedule with key details like wake times, medication instructions, and preferred activities to maintain consistency. Tools like shared online calendars can also make it easier for friends and family to commit to specific time slots. Instead of a general request like, "Can you help with Mom?" try asking, "Can you sit with her for one hour on Tuesday afternoon?" Having a clear task list ready makes it easier to ask for and receive help when you need it.
Taking these breaks isn’t just about recharging – it’s about ensuring you’re able to continue being there for your loved one in the long run.
Maintain Your Own Health and Balance
Keep an eye out for signs of burnout, such as constant fatigue, irritability, withdrawing from social activities, skipping meals, or losing interest in things you used to enjoy. Caregivers are also less likely than others to schedule regular checkups, so make it a point to prioritize your own health. Aim for 7–9 hours of sleep, eat balanced meals, stay hydrated, and try to fit in at least a 15-minute walk each day.
You can also incorporate small moments of mindfulness into your daily life. For example, take a few deep breaths while washing dishes or waiting at a red light. Joining a caregiver support group – whether online or in person – can provide a sense of community and help you manage stress. Additionally, inform your primary care doctor about your caregiving role; they may be able to connect you with resources like mental health counselors or support services.
Conclusion
Creating a daily care routine for your aging parent doesn’t have to feel like an impossible task. By following the seven steps – assessing needs, planning a schedule, focusing on essential care, prioritizing safety, coordinating help, staying adaptable, and taking care of yourself – you’re setting up a system that supports everyone involved. Routines aren’t about strict rules; they’re about providing structure and stability, serving as a guide rather than a constraint. These steps work together to create a solid foundation for successful caregiving.
Predictable routines can ease anxiety and reduce confusion, offering seniors a sense of security and control. Activities like puzzles or social interactions can keep the mind sharp, while regular sleep patterns help regulate the body’s internal clock for better rest. Even small efforts make a difference – just 11 minutes of moderate exercise each day can reduce the risk of early death by 23%.
A well-thought-out caregiving routine brings calm to what can often feel chaotic. It promotes emotional stability, encourages independence, and reduces decision fatigue for both caregivers and seniors. Start reaping these benefits by taking small but meaningful steps today.
For extra support, consider using the ElderHonor Toolkit. It includes over 30 checklists and worksheets to help you evaluate your parent’s needs, share caregiving duties with family, and create a personalized plan.
Start small and stay flexible – every routine you establish today makes tomorrow a little easier.
FAQs
How can I evaluate my parent’s ability to manage daily tasks?
To understand your parent’s ability to manage everyday tasks, focus on two main categories: Activities of Daily Living (ADLs) – like bathing, dressing, eating, and moving around – and Instrumental Activities of Daily Living (IADLs), which include tasks such as managing medications, cooking, and handling finances. These areas can give you a clear picture of their independence and highlight where they may need help.
Start by observing how they handle these activities over a few days. Pay attention to whether they can complete tasks on their own, need occasional assistance, or require full support. You can also ask direct questions, such as “Are you able to prepare a simple meal by yourself?” or “Do you feel comfortable keeping track of your medications?” Keeping notes over time can help you spot patterns or changes in their abilities.
If you prefer a more structured method, tools like checklists or questionnaires can be very helpful. For example, resources like the ElderHonor Toolkit offer step-by-step guidance for evaluating daily abilities and creating tailored care plans. This approach ensures your parent’s safety and well-being, while also honoring their independence.
How can I make my home safer for my aging parent?
Creating a secure and comfortable home for seniors often starts with a few practical adjustments to minimize the chances of falls and accidents. For example, you can install grab bars near the toilet and in the shower, place non-slip mats in the bathroom, and keep walkways free of loose rugs, cords, or other clutter. Simple additions like night-lights in hallways and bathrooms can make a big difference in visibility, while features like lever-style handles and wider doorways can help those with limited mobility move around more easily.
Technology can play a big role in enhancing safety, too. Devices like medication reminders, smart-home sensors that monitor unusual activity, and emergency response systems – such as wearable panic buttons or fall-detection pendants – can provide extra peace of mind. If stairs are a concern, installing a stair lift or ramps can help make the home more accessible. These changes not only create a safer living space but also help seniors maintain their independence and confidence.
What are some tips for caregivers to prevent burnout while managing a senior’s daily routine?
Preventing burnout starts with crafting a routine that’s balanced and manageable, ensuring both the senior’s needs and the caregiver’s well-being are addressed. Focus on the essentials – like preparing meals, managing medications, maintaining hygiene, and incorporating light physical activity. Keeping the schedule straightforward can help minimize feelings of being overwhelmed. Be sure to include short breaks for yourself and the senior, and stay adaptable to handle any unexpected changes with ease.
Involve the senior in small, suitable tasks, such as folding laundry or setting the table. These activities can give them a sense of purpose while also lightening your workload. Carve out time for meaningful shared moments, like enjoying a cup of tea together or watching a favorite show. These interactions not only strengthen your bond but also provide emotional support for both of you.
Taking care of yourself is just as important. Set aside at least 30 minutes daily for activities that help you unwind – whether it’s a walk, reading a book, or meditating – and treat this time as non-negotiable. If stress starts to mount, don’t hesitate to reach out for help, whether from a neighbor, respite care services, or a support group. Resources like the ElderHonor Toolkit can also provide valuable guidance and tools to navigate caregiving challenges. Regularly reviewing and adjusting the routine ensures it remains practical and helps ward off burnout.

